This recent news article discusses a new candidate antimicrobial called Globomycin and the work that researchers at Trinity College Dublin have put in to map out its spatial organization. A particularly interesting point that is discussed is the idea of narrow-spectrum antibiotics. Antibiotic/antimicrobial resistance is driven in part by the fact that these drugs target a broad range of microbes, killing off those that don’t necessarily need to be killed, thus providing possible niche-space for pathogens and the like that survived the drug. A narrow-spectrum antibiotic would be more specifically targeted to one or a few microbes that we particularly want to eradicate.
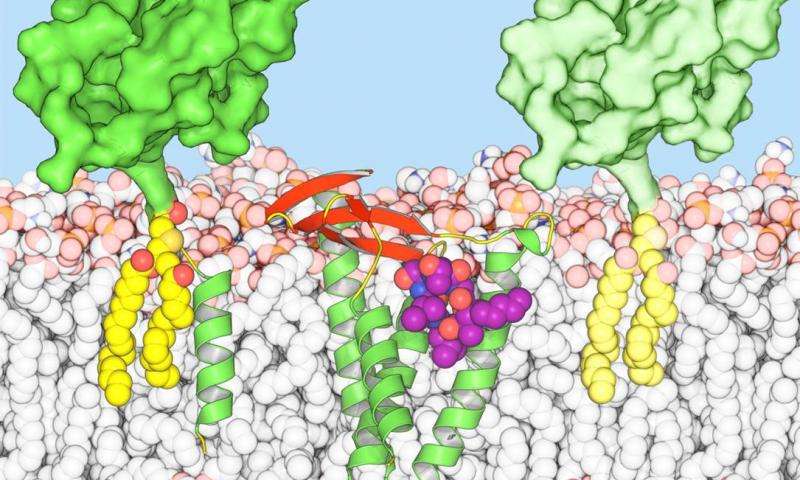
The hope is that Globomycin’s structure will aid in producing a whole suite of new antimicrobials with a species-specific target. This specificity will theoretically decrease antibiotic resistance (although nature always seems to find a way…). Although this would be a great achievement in battling resistance, I still personally think we should continue to use antimicrobials and antibiotics only when necessary. I’m worried that new antimicrobials will trick people (particularly policy makers) into thinking they can continue to use these drugs irresponsibly and that the recent bans on antimicrobials in agricultural settings will no longer be seen as necessary. I don’t think new antimicrobials that are less susceptible to resistance is a bad thing – just a tool in a larger set, to be combined with other antimicrobial stewardship practices as opposed to a singular remedy.