There are a bunch of stories starting to come out based on some press and paper releases from the CDC yesterday. One that seems well done is this from CIDRAP: CDC notes progress, threat regarding hospital superbugs | CIDRAP.
Today’s CDC report focused on the six most concerning antibiotic-resistant bacteria and found better progress against them in short-term healthcare settings.
Basically, there is some good news and some bad news.
The good news:
Hospital acquired infections in acute care hospitals are showing some improvements:
- “A 50 percent decrease in central line-associated bloodstream infections (CLABSIs) between 2008 and 2014.”
- “A 17 percent decrease in surgical site infections (SSIs) between 2008 and 2014 related to 10 procedures tracked in previous HAI progress reports.”
- “No change in the overall catheter-associated urinary tract infections (CAUTIs) between 2009 and 2014. During this time, however, there was progress in non-ICU settings, progress in all settings between 2013 and 2014, and most notably, even more progress in all settings towards the end of 2014.”
- “CDC’s annual progress report shows that progress has been made in decreasing hospital-onset C. difficile infections by 8 percent between 2011 and 2014.”
Ok so #3 of those above is not so much good news, but it is maybe neutral. But then the bad news
But then the bad news:
- “In acute care hospitals, 1 in 7 catheter- and surgery-related HAIs can be caused by any of the six antibiotic-resistant bacteria listed below. That number increases to 1 in 4 infections in long-term acute care hospitals, which treat patients who are generally very sick and stay, on average, more than 25 days. The six antibiotic-resistant threats examined are:
- Carbapenem-resistant Enterobacteriaceae (CRE)
- Methicillin-resistant Staphylococcus aureus (MRSA)
- ESBL-producing Enterobacteriaceae (extended-spectrum β-lactamases)
- Vancomycin-resistant Enterococcus (VRE)
- Multidrug-resistant Pseudomonas aeruginosa
- Multidrug-resistant Acinetobacter”
- “1 in 6 remaining CLABSIs are caused by urgent or serious antibiotic-resistant bacteria.”
- “1 in 7 remaining SSIs are caused by urgent or serious antibiotic-resistant bacteria.”
- “1 in 10 CAUTIs are caused by urgent or serious antibiotic-resistant bacteria.”
So that is kind of scary. What can we do? They say:
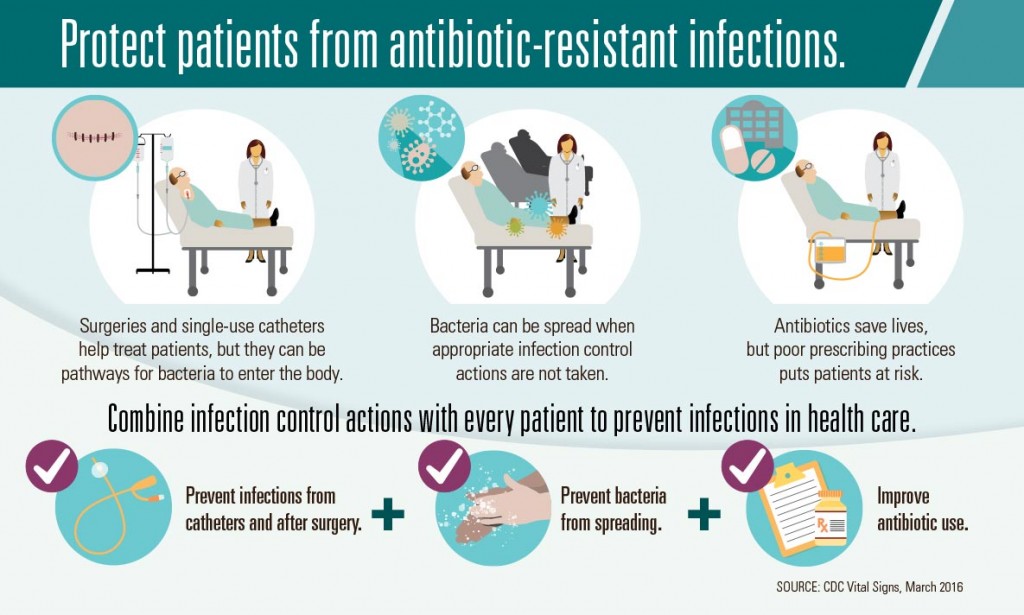
- CDC is calling on doctors, nurses, health care facility administrators, and state and local health departments to continue to do their part to prevent HAIs. The report recommends doctors and nurses combine three critical efforts to accomplish this:
- Prevent the spread of bacteria between patients;
- Prevent infections related to surgery and/or placement of a catheter; and
- Improve antibiotic use through stewardship.
“For clinicians, prevention means isolating patients when necessary,” said Clifford McDonald, M.D., Associate Director for Science at CDC’s Division of Healthcare Quality Promotion. “It also means being aware of antibiotic resistance patterns in your facilities, following recommendations for preventing infections that can occur after surgery or from central lines and catheters placed in the body, and prescribing antibiotics correctly.”
I don’t know about you but this does not overwhelm me as a plan since, well, who knows if people will follow this. Fortunately, the CDC got some $160 million extra related to the National Action Plan for Combating Antibiotic-resistant Bacteria. And with this money they plan to:
- accelerating outbreak detection and prevention in every state;
- enhancing tracking of resistance mechanisms and resistant infections;
- supporting innovative research to address current gaps in knowledge; and
- improving antibiotic use.
Oh, and they made some nice infographics about the topic:
UPDATE 3/4/16 & 3/5/16
Some more coverage of the CDC releases
- Oregon Live: CDC: Superbugs cause 1 in 7 infections caught in hospital
- UPI: CDC: Hospitals making progress against ‘superbugs’
- “To combat the problem of antibiotic-resistant infections, the CDC is calling on doctors, nurses and hospital staff to continue to prevent the spread of bacteria between patients. The CDC is also asking healthcare professionals to reduce infections related to surgery and placement of catheters. The agency is also calling for cautious use of antibiotics to help fight resistance.“
- NBC News America’s Germiest Hospitals? The Answer May Surprise You
- USA Today by Liz Szabo: Rates of some hospital-acquired infections fall by 50%
- “Americans developed 722,000 infections related to health care in 2011, according to a report released Thursday by the Centers for Disease Control and Prevention. Such infections wouldn’t have developed if people hadn’t gone to a hospital or nursing home. About 75,000 patients with these infections died.”
- Arizona Daily Star: Arizona hospital infections drop, but superbugs still pose threat
- Maryn McKenna at Germination: Some US Hospital Infections Dropping, But Superbug Risks Are High. Some quotes below:
- In a phone briefing with reporters, Dr. Thomas Frieden, the CDC’s director, called the high levels of resistance in infections in long-term care facilities–more than one in four of each infection– “chilling.” Asked how he would describe the rate in regular hospitals, which exceeds one in seven, he replied: “deeply concerning.”
- Dr. Peter Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins–an early champion of cockpit-style checklists to prevent healthcare infections, who was also on the call to reporters–added: “We need things to better identify organisms faster, so we could implement appropriate checklists. We need to better understand when surfaces are clean very much earlier, so we know if our cleaning efforts are effective. And we need to have better regional and networked information systems, so we know what resistance patterns are in community hospitals and longterm care facilities, and be able to link them when patients come to acute-care hospitals and then go back again.”
- Mike the Mad Biologist: An Atlas Of Antibiotic Resistance
And some Twitter posts of possible interest
New #VitalSigns focuses on connection between #antibiotic-resistant bacteria & healthcare-associated infections https://t.co/mTAc6GkSfP
– Dr. Tom Frieden (@DrFriedenCDC) March 3, 2016
On any given day, 1 in 25 hospital patients has at least one healthcare-associated infection that they did not come in with. #VitalSigns
– Dr. Tom Frieden (@DrFriedenCDC) March 3, 2016
Of 18 #antibiotic-resistant bacteria identified as health threats in 2013 by CDC, nearly half cause healthcare-associated infections.
– Dr. Tom Frieden (@DrFriedenCDC) March 3, 2016
Prevent spread of bacteria btwn patients. Prevent infections related to catheters, surgeries. Improve antibiotic stewardship. #VitalSigns
– Dr. Tom Frieden (@DrFriedenCDC) March 3, 2016
Links to the CDC releases
- Vital Signs: Preventing Antibiotic-Resistant Infections in Hospitals – United States, 2014
- Press release: Superbugs threaten hospital patients
- CDC’s Antibiotic Resistance Patient Safety Atlas
Other Material from CDC
- HAI Data and Statistics
- HAI prevention progress and activity in your state
- HAI Progress Report FAQ
- Patient Safety: What you can do to be a safe patient
- Preventing HAIs.
- HAI Prevention Toolkits
- Targeted Assessment for Prevention (TAP)
Also of interest/relevance:
- National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination
- Understanding the Role of Facility Design in the Acquisition and Prevention of Healthcare-Associated Infections from HERD Journal
- Infection Control and 
the Built Environment: 
No Easy Answers
- Moving toward elimination of healthcare-associated infections: A call to action
- Approaches for Preventing Healthcare-Associated Infections: Go Long or Go Wide?
- Advances in the Prevention and Control of HAIs – by AHRQ
- Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. PDF.

Regarding “prevent bacteria from spreading:”
1. Nothing about testing and improving air filtration to capture particles of the sizes of the known infectious agents.
2. Nothing about the risk factors for patient to patient or patient to HCW transmission —
* crowding, e..g., patients too close together or too many in a confined space
* inadequate ventilation rates,
* improper directional flow of air associated with infected and susceptible patients.
* inappropriate design and or maintenance (e.g., lamp replacement) of UVGI systems
* ineffective triage of potentially infectious patients upon entering the healthcare facility
3. Nothing about the nature and use of antibiotic or sterilization products on instruments and surfaces.
What do all of these have in common? They all implicate the healthcare facility, There are large financial implications when infected former patients or their estates file law suits against hospitals and other healthcare facilities. Wrongful death suits are expensive, and these have been seen following a documented case of Legionnaire’s Disease in a building (including a healthcare) or other facility.
Hal
I agree that the plan discussed starting at “CDC is calling on doctors …” is limited.
However, though I cannot speak for the CDC here, my guess is they would say some of the topics you write about covered in the last four things I list: accelerating outbreak detection and prevention in every state; enhancing tracking of resistance mechanisms and resistant infections; supporting innovative research to address current gaps in knowledge; and improving antibiotic use.
Jonathan:
Guess as much as you like. It would be a good idea if your guesses were better informed. You can find CDC’s guidance documents on the web if you care to reduce the guesswork in your comments. For example, check out http://www.cdc.gov/coronavirus/mers/infection-prevention-control.html. or http://www.cdc.gov/coronavirus/mers/infection-prevention-control.html. there are lots more documents there that are easily accessible and not behind a paywall.
I have been involved with the WHO and CDC and elsewhere on this topic, and I am not guessing. Your comments evokes anger since you really don’t know what you are talking about, but you try to cover your possible errors with the caveats, well, and “my guess here is….” Why do you bother to post if you are just guessing?
To the extent that the measures I mentioned are covered by the CDC, they are only covered in such a general way in your post as to fail to communicate the importance of the detailed actions required to complement hand-washing which is the only specific item they identify. I think my point that it is typical in modern hospitals aggressively and broadly to promote hand[washing as a way to put the responsibility on individuals — visitors, patients, and doctors. this detracts us from the things the facility can do to help. I do not see anything that you said that addresses that fundamental point.
You can find CDC’s guidance documents on the web if you care to reduce the guesswork in your comments.
I am not guessing and will not apologize or caveat my comments. It is very clear to me in healthcare facilities in America and, to some extent, elsewhere, that the facilities are obsessed with reducing their liability and they are being sued for and paying huge settlements to affected patients and their estates. It’s all about money!
Every years for the last several (maybe 6) years, I have been teaching part of a 2-week course on Airborne Infection Control in healthcare facilities at Harvard School of Public Health and Harvard Medical School. It is organized by Ed Nardell from the faculty of those two Harvard schools and by Paul Jensen from the CDC. Jensen travels the globe to help advise healthcare facility operators on what they can do to reduce airborne disease transmission. Nardell is one of the world’s foremost experts on TB prevention and treatment. He developed the course with assistance from WHO in Geneva.
The focus in the course is on control of airborne disease transmission through facility design, operation, and management. The course goes beyond what the CDC guidance provides and, for that reason, CDC is now supporting the course. The focus is on the facility and the approaches available beyond what the CDC message conveys. The students are doctors, facility managers, architects and engineers who are responsible for facilities around the world although mostly in Africa. Most of the students’ facilities do not even have electricity. But they come because they need to know what can be done in such resource-scarce situations.
I also was an external reviewer and part of the group that formulated the WHO guidelines on natural ventilation in healthcare facilities to prevent airborne infectious disease transmission. (available for free download — no paywall — at http://www.who.int/water_sanitation_health/publications/natural_ventilation.pdf).
My focus is clearly different from yours, and clearly clearer than yours based not on guesswork but on experience and knowledge relevant to the subject at hand.
Hal
I welcome your ideas and critiques. But I do not believe making your critiques personal is appropriate for this site.
I note – I stand by my original post. I think it was useful to point people to the CDC and CIDRAP releases. One of our jobs here at microBEnet is to share information about what is being written about in regard to microbiology of the built environment. When I write blog posts my goal is not to necessarily editorialize about everything. Sometimes I think it is better to be indirect. I wrote “I don’t know about you but this does not overwhelm me as a plan …” in order to at least put the idea in people’s heads that this plan was imperfect.
I get you do not like that approach. Your ideas are welcome and critiques too though I believe you are overreacting to a response I made to your comment (it is a blog after all and I was responding to your comment with some speculation). But please Hal keep the comments about the science and avoid personal attacks, they are not welcome here. This appears to be a recurring theme with some of your comments and in most other cases they are targeted towards students writing blog posts. This is a site with a major goal in building community. And your tone and personal attacks are not helping in that regard.
I really hate to clutter up this site with this thread but I guess I do want to follow up on Hal’s comments in one regard.
I decided to look around to see if my “guess” comment he disliked so much had any support. And, well, it does. Here is the guess comment:
” I cannot speak for the CDC here, my guess is they would say some of the topics you write about covered in the last four things I list: accelerating outbreak detection and prevention in every state; enhancing tracking of resistance mechanisms and resistant infections; supporting innovative research to address current gaps in knowledge; and improving antibiotic use.”
I guess the reason I wrote this was that Hal’s original comment implied that he believed the CDC was not including all these other topics Hal listed because they were less concerned about patient safety and more concerned about preventing lawsuits against hospitals. He wrote:
“What do all of these have in common? They all implicate the healthcare facility, There are large financial implications when infected former patients or their estates file law suits against hospitals and other healthcare facilities.”
Since this seemed to be an attack against the CDC I guess I responded by saying my guess is the CDC would say that they are not ignoring patient safety but that they are addressing these topics in some way. I was not (and still am not) trying to defend the CDC and I note I even agreed with Hal that the plan was limited. I guess I was simply saying I thought they would likely say they are covering these areas in some way. And, well, fitting my guess (though again, I don’t know what the CDC would say), it was easy to find CDC documents that covered many/most of the topics Hal mentioned as being neglected. Examples are below:
http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5210a1.htm
http://www.cdc.gov/MMWr/preview/mmwrhtml/mm63e1114a3.htm
http://www.cdc.gov/HAI/settings/outpatient/basic-infection-control-prevention-plan-2011/transmission-based-precautions.html
http://www.cdc.gov/biosafety/publications/bmbl5/BMBL5_sect_IV.pdf
http://www.cdc.gov/HAI/prevent/top-cdc-recs-prevent-hai.html
http://www.cdc.gov/hai/organisms/cdiff/Cdiff_clinicians.html
http://www.cdc.gov/niosh/docs/2009-105/
http://www.cdc.gov/hicpac/Disinfection_Sterilization/3_4surfaceDisinfection.html
http://www.cdc.gov/HAI/prevent/sd_medicalDevices.html
http://www.cdc.gov/HAI/organisms/hiv/hiv.html
http://www.cdc.gov/HAI/prevent/sd_medicalEquip.html
And others. So I again would guess that the CDC would say they are not ignoring these areas and that they are not part of some conspiracy to protect hospitals from lawsuits. My guess is this would not appease Hal in any way. But I guess that is going to have to do. And again, apologies for the clutter.
Those infographics are really great. I hope they make their way into more hospitals. Feels like something like this should have existed earlier to bridge the gap between what researchers know about antibiotic resistance and what doctors practice in clinics. Maybe it does exist, but I sure haven’t seen antibiotic resistance addressed in the hospitals I’ve been to recently.
At the launch conference of the Network for Anti-Microbial Resistance and Infection Prevention (NAMRIP) in Southampton, UK, Professor Bill Keevil – Chair in Environmental Healthcare at the University of Southampton – addressed the question ‘Can we prevent bacteria having sex on a surface and transferring their antibiotic genes?’
Highlighting the rise of ‘superbugs’ and inadequacies in hand washing, he covered his work at the university looking at the role of touch surfaces in the spread of infection.
Horizontal gene transfer (HGT) in bacteria plays an important role in the evolution of antibiotic-resistance, which has led to an increasing number of difficult-to-treat healthcare-associated infections.
Professor Keevil’s research shows that, while HGT can take place in the environment – on frequently-touched surfaces such as door handles, trolleys and tables from stainless steel – copper prevents this process from occurring and rapidly kills bacteria on contact.
Professor Keevil’s presentation concluded that a combination of effective cleaning regimes, and touch surfaces made from antimicrobial copper, could be invaluable in preventing the spread of pathogens and antimicrobial resistance.
Video of Professor Keevil’s presentation: https://www.youtube.com/watch?v=adZIsecwgmk&index=7&list=PLdoU820Bg57d3O3BDe9IsF4MDclggWYyd
NAMRIP website: http://www.southampton.ac.uk/namrip/index.page?
Information site about copper surfaces: http://www.antimicrobialcopper.org
Andrew – I appreciate the comments. However I think it is important for people to know – you work for a company that markets “antimicrobial copper touch surfaces” http://www.act-surfaces.co.uk. I am guessing, but could not find further information to support this, that Bill Keevil has some role in your company. I note – I am skeptical of many of the claims made by companies promoting antimicrobial surfaces including those made of copper.