“Should we always antibiotics until the end of their course?”
Well, this has been a question asked on and off over the last 10 years or so. And this I was quite interested in a Tweet I saw from Eric Topol this AM (I note – Eric Topol on Twitter is a better source of information about interesting new health – related studies than just about anyone or anything out there)
Challenging medical dogma on antibiotics https://t.co/cUkJMxlnTX @bmj_latest #OAhttps://t.co/MfS9nmflFQ @sarahboseley @guardianscience pic.twitter.com/xbU6uSolKh
— Eric Topol (@EricTopol) July 30, 2017
So I went to the commentary that he linked to in BMJ: The antibiotic course has had its day | The BMJ. It is a commentary written by Martin J Llewelyn, professor of infectious diseases, Jennifer M Fitzpatrick, Elizabeth Darwin, SarahTonkin-Crine, Cliff Gorton, John Paul, Tim E A Peto, Lucy Yardley, Susan Hopkins. And indeed they concludes that, no, we unquestionably should not always finish a course.
The short summary is as follows:
With little evidence that failing to complete a prescribed antibiotic course contributes to antibiotic resistance, it’s time for policy makers, educators, and doctors to drop this message, argue Martin Llewelyn and colleagues.
I note – if you are interested in the history of the paper, BMJ has released the full peer review history including names of reviewers. It makes for an interesting read. I wish more and more journals would open up their peer review like this. If you want to read the article it is at least freely available for now (not sure if it is truly Open Access or when it may not be free) but good that it is available now. The paper is worth a read.
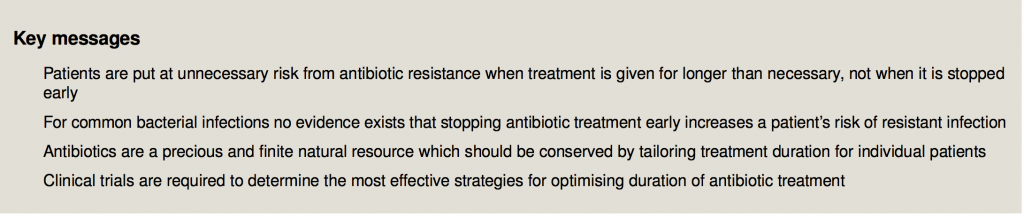
Some of their key points are summarized in this Box
Also the last section of the paper seems particularly key:
What should we advise patients?
The “complete the course” message has persisted despite not being supported by evidence and previous arguments that it should be replaced.18 38 One reason it may be so resilient is that it is simple and unambiguous, and the behaviour it advocates is clearly defined and easy to carry out. Nevertheless, there is evidence that, in many situations, stopping antibiotics sooner is a safe and effective way to reduce antibiotic overuse. Daily review of the continued need for antibiotics is a cornerstone of antibiotic stewardship in hospitals,39 but in primary care, where 85% of antibiotic prescriptions are written, no such ongoing assessment is attempted.
There are reasons to be optimistic that the public will accept that completing the course to prevent resistance is wrong if the medical profession openly acknowledges that this is so, rather than simply substituting subtle alternatives such as “exactly as prescribed.” Completing the course goes against one of the most fundamental and widespread medication beliefs people have, which is that we should take as little medication as necessary.40 Concerted and consistent efforts have successfully educated the public that antibiotics do not treat viral infections, for example.
Research is needed to determine the most appropriate simple alternative messages, such as stop when you feel better. Until then, public education about antibiotics should highlight the fact that antibiotic resistance is primarily the result of antibiotic overuse and is not prevented by completing a course. The public should be encouraged to recognise that antibiotics are a precious and finite natural resource that should be conserved. This will allow patient centred decision making about antibiotic treatment, where patients and doctors can balance confidence that a complete and lasting cure will be achieved against a desire to minimise antibiotic exposure unimpeded by the spurious concern that shorter treatment will cause antibiotic resistance.
If you want an alternative view of the paper there are some news stories about it worth checking out
- Sarah Boseley in the Guardian: Rule that patients must finish antibiotics course is wrong, study says
- San Diego Tribune Taking antibiotics for full 7 to 14 days can actually harm you
There has also been some pushback. A good example is in an article in Gizmodo: Doctors Slam New Recommendation That We Should Stop Antibiotic Treatments Early. This includes some useful comment sand caveats including:
- Michael Baym.
- That said, Baym says that replacing the general advice to finish a course with general advice to not finish a course is likewise based on insufficient evidence.“I think the real conclusion is that we need to get away from the idea that all antibiotics and all infections require uniform thinking, and instead do specific studies to find out ideal treatment regimens for specific infections and specific antibiotics,” Baym told Gizmodo.
- Haha Farhat
- Maha R. Farhat, Assistant Professor of Biomedical Informatics at Harvard Medical School, agrees with Baym, saying the authors made an ambitious statement that isn’t currently founded in sufficient evidence. “Most infectious disease doctors and antibiotic resistance specialists would like to see less use of antibiotics but the reality is that we we don’t yet have enough evidence to throw a blanket statement as the authors did,” Farhat told Gizmodo. “It’s true that collateral resistance is an issue, but what this should call for is more research and not a premature change in public health recommendations and awareness campaigns as the authors suggest.”
- Vaughn Cooper
- Vaughn Cooper, a microbiologist at the University of Pittsburgh School of Medicine, says we most certainly need to reconsider the the “one-size-fits-all” approach to antibiotic prescriptions, but he describes the new editorial as being “clearly dangerous.”“Arguing that antibiotic course duration is not sufficiently evidence-based is worthwhile, but the editorial essentially argues that patients should not finish their course of antibiotics,” Cooper told Gizmodo. “This, too, is not evidence-based and increases the likelihood of adverse outcomes for patients disregarding medical advice when a course of antibiotics is clearly warranted.”
- and more.
So – it looks like there is no consensus on whether there should be new recommendations to patients.
There is less evidence provided hence more research is needed.
Antibiotic use is required to overcome bacterial infection. Dosage and duration of the course depends on body weight of the patient and severity of the infection. Completing the course makes sense for the purpose of ensuring the bacterial infection is no longer there, which is possible if the right antibiotic is used and the minimum inhibitory concentration is achieved. Completing the course has not much relevance for preventing antibiotic resistance but from point of view of infection control it still makes sense perhaps.